Posted 4 years ago
Breast Cancer Screening in the Transgender Population
We all rely on health care services at some point in our lives, and often these services are taken for granted. Unfortunately, not everyone has equal access to medical advice and treatment. This disparity is highlighted among the LGBTQIA+ population. In 2016, the LGBTQIA+ community was identified by the National Institute on Minority Health and Health Disparities as a “health disparity population.” LGBTQIA+ individuals span all race, ethnic, religious, and social spectrums. A 2017 survey of LGBTQIA+ people conducted by the Center for American Progress reported that nearly 1 in 10 LGBTQIA+ individuals reported that a health care professional refused to see them in the prior year because of their actual or perceived sexual orientation. Despite the lack of data on cancer rates within the LGBTQIA+ community, the National LGBT Cancer Network reports that LGBT communities are disproportionately affected by cancer.
According to Centers for Disease Control, approximately 1 million people in the United States identify as transgender. Transgender is an umbrella term applied to individuals whose gender identity and/or gender expression differs from their gender assigned at birth (natal sex). Gender identity is defined as the innate identification of gender as male, female, or somewhere else on the gender spectrum and may not correspond to external anatomy. Gender expression is defined as intentional and unintentional manifestations of a person’s gender identity (physical appearance, behavior, and presentation).
With an increasing number of individuals undergoing gender-affirming hormone therapy and gender-affirming surgery, the population within the US that identifies as transgender is anticipated to rise over the coming years. Transgender individuals have reported difficulties within the US health care system: 19% have reported refusal of care, 28% reported harassment, and 50% report that they were turned off by the healthcare system due to a lack of gender non-conforming providers. Many transgender patients only seek medical care as a part of a gender affirmation and may avoid primary health care concerns. Patients that do seek routine healthcare appointments are sometimes reluctant to share gender incongruous organs. Therefore, transgender patients may be more reliant on their health care provider to initiate cancer screening discussion than cis-gender patients. It is important to recognize the health-care disparities faced by this community and be aware of the specific cancer screening recommendations for this population.
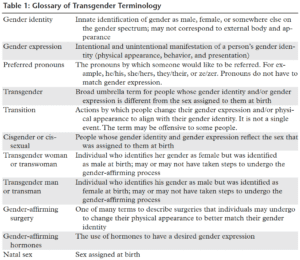
In order to provide care for the transgender population, physicians must embrace the patient’s self-identification, be aware of their specific medical needs, and create a welcoming and safe practice. An essential step in developing and maintaining doctor-patient trust is to greet and address the transgender patient by using the appropriate and preferred terminology. A glossary of transgender terminology is provided in Table 1. There are several other references available with glossaries of terms including the Gay and Lesbian Alliance Against Defamation (GLAAD) Medial Reference Guide and the Fenway Health Glossary of Gender and Transgender Terms. Use of the correct terminology with patients indicates that the provider is making an effort to be inclusive. As an overarching rule, care should be taken to ask the patient for their preference in terminology and pronouns.
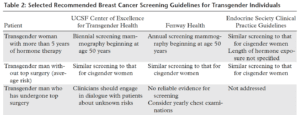
The American Cancer Society (ACS) and US Preventive Services Task Force (USPSTF) and numerous other professional organization (ACS, AMA, AUA, ACOG) have clear recommendations for the early detection of cancer in average-risk and high-risk cis-gender patients. There is no doubt that these guidelines become less straight forward when applied to the transgender community; however, every effort should be made to provide optimal cancer screening for the transgender patient. The information that follows will focus specifically on the recommendations for breast cancer screening in the transgender population as delineated by the University of California San Francisco Center of Excellence for Transgender Health and Fenway Health.
Many transgender women use feminizing hormones to undergo gender affirmation. Generally, this involves the use of estrogen and antiandrogen medications to suppress endogenous testosterone. Hormonal changes include breast growth, slowed growth of body and facial hair, fat redistribution, and decreased testicular size. Maximum breast growth usually occurs at 2-3 years after the start of hormone therapy. As a result, a spectrum of breast density levels are seen mammographically. Histologically, transgender women taking gender affirmation hormones develop breast tissue that is similar to that of cisgender women with ducts, lobules, and acini. Because hormonally-driven breast tissue development in transgender women is similar to that of cisgender women, similar benign and malignant lesions have been found in transgender women.
Given the relationship between exogenous hormone therapy and the risk of breast cancer, screening mammography has been recommended in the transgender female population. Because current recommendations are largely based upon the screening guidelines for cisgender women, there is a lack of uniformity among guidelines. Current screening guidelines vary according to age of the individual and risk factors including duration of hormone therapy. Generally, it is recommended to start screening annually or biennially staring at age 50 years. Table 2 provides recommendations for breast cancer screening in transgender individuals.
Written by
Resident Andrew S. Brown, DO (not affiliated with Ironwood Cancer & Research Centers)
and Emily Ho, MD, MS
Glossary click here.