Posted 7 months ago
Thyroid Cancer Awareness
The month of September is Thyroid Cancer Awareness Month. It is important to note that over 60,000 people will be diagnosed with thyroid cancer this year in the United States. The yearly incidence of thyroid cancer has nearly tripled since 1975, with almost all of the increase is due to papillary thyroid cancers. The increase in diagnosis is likely due to improved imaging techniques and our ability to find cancer much earlier. Thyroid ultrasound is a means of detecting abnormal nodules within the thyroid. Most thyroid nodules are benign and can be followed with serial imaging every six months to 1 year. However, suspicious nodules need to be biopsied to confirm the presence of cancer.
There are several different types of thyroid cancer, including anaplastic carcinoma, medullary carcinoma, and well-differentiated thyroid cancers (papillary, follicular, and Hurthle cell). Anaplastic and medullary carcinomas are rare forms of thyroid cancer that are very aggressive with a high risk of metastatic disease. Thankfully, well-differentiated thyroid cancers such as papillary and follicular carcinoma, which account for >90% of all thyroid cancers, are very treatable with an excellent prognosis.
Typically, treatment consists of surgery to remove the thyroid gland, called a thyroidectomy. The treatment plan for some patients after surgery can include radioactive iodine treatment, also known as RAI therapy. However, not everyone with thyroid cancer needs to undergo RAI treatment. Recent changes in guidelines have allowed us to avoid treatment in most low-risk patients, or treat with a much lower dose of RAI and thus reduce potential side effects and late-term complications of treatment.
Low-risk patients typically have a less than 5% risk of developing a recurrence of cancer. Intermediate risk patients anywhere from 5-15% risk of recurrence and high-risk patients generally are higher than 20-30% risk of recurrence. RAI therapy after surgery can reduce the risk of recurrence by 3-4 fold. However, treatment can come with side effects that may include fatigue, taste changes, dry mouth, dry eyes, nausea and indigestion, low blood counts, and even the risk of secondary cancers in the future. Most of the side effects are temporary but can be permanent in a small percentage of patients.
A recent study published in the journal Surgical Oncology, by Willis et al., showed that approximately 25% of patients with low risk and well-differentiated thyroid cancer received RAI treatment that guidelines do not recommend. Over-treatment of low-risk thyroid cancer is of serious concern. In my opinion, it is very important for patients to undergo a full consultation and evaluation of their case to determine the stage of their cancer and level of risk of recurrence by a board-certified radiation oncologist. I am personally committed to following the American Thyroid Association guidelines for RAI therapy, to minimize exposure of radiation to patients unnecessarily.
I am a firm believer in what is called shared decision-making. Patients should feel as though they have a choice in their treatment decision. This is why thyroid cancer awareness is important. It is imperative for physicians to take the time necessary to explain the risks and benefits of treatment and allow patients the opportunity to be involved in the decision-making process. A patient should never feel that they are being pushed toward a treatment that they don’t want or understand.
One important thing to remember during thyroid cancer awareness month is that most thyroid cancers have a good prognosis and are highly curable if caught early. At Ironwood Cancer & Research Centers Center we do our best to make sure that patients understand their treatment options and become involved in the decision making the process. There is a great deal of fear and anxiety that comes along with a thyroid cancer diagnosis, but with early detection and modern advancement in treatment technology along with proper patient education and appropriate care, excellent treatment outcomes are likely.
Dr. Davis Romney
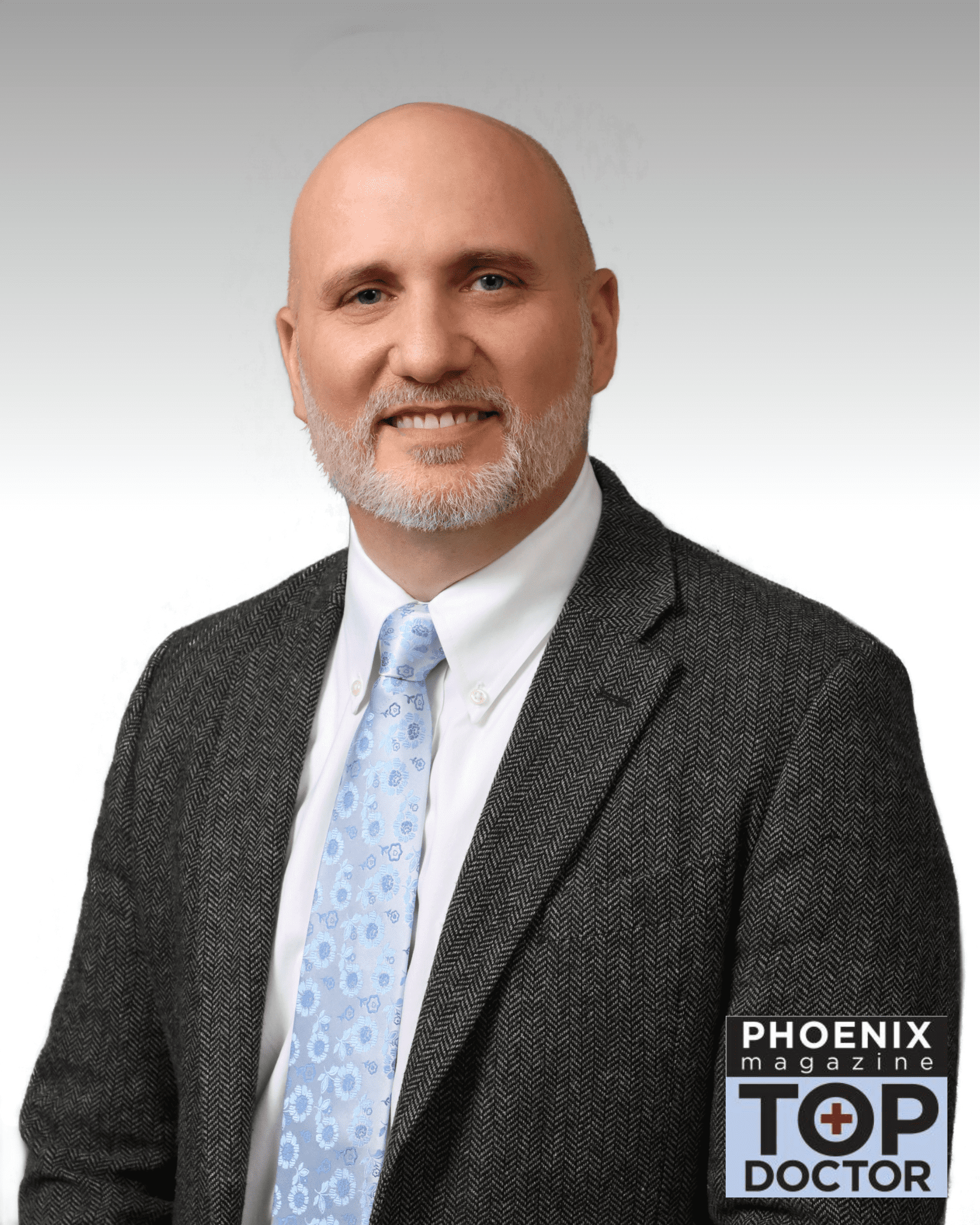
He is trained and experienced in 3-D conformal radiation therapy, IMRT, IGRT, SBRT, TomoTherapy, GammaKnife, and I131 thyroid ablation, as well as LDR and HDR brachytherapy, including prostate seed implants and breast brachytherapy. Dr. Romney is board certified in Radiation Oncology by the American Board of Radiology, specializing in breast, gynecologic, lung, head & neck and thyroid malignancies. He has been selected by his professional peers as a Top Doc in PHOENIX Magazine.
He is married to his wife, Tanja, and they have 5 children. In his free time, Dr. Romney enjoys spending time with his family, playing softball, running marathons, traveling, and participating in this children’s school and recreational activities.